Disclosure: This post may contain affiliate links, meaning, at no additional cost to you, I may earn a commission if you click on, or make a purchase through a third-party link.
A migraine is a severe headache, often accompanied by nausea, vomiting, and light sensitivity. These headaches may last from four hours to several days. The American Migraine Foundation estimates that migraines occur in 1 billion people worldwide. Migraine affects adult women about 3.25 more often than men.
This is likely the result of hormone fluctuations occurring in females. The fact that prepubertal children have a migraine incidence of 3-10% regardless of gender also supports the theory that hormones play a role.
The incidence of migraines remains relatively equal in boys and girls until the age of nine. After nine, more girls experience these headaches.
It is known that estrogen is able to cross the blood-brain-barrier freely. Obese women have a higher risk of developing migraines. This is thought to be due to increased estrogen production in the adipose tissue.
Migraine headache ranks seventh globally for years lived with disability.

Migraine Aura Triggers
In fifteen to thirty percent of migraine sufferers, an aura precedes the headache pain.
This is most commonly visual but may be a disturbance of speech or motor function as well. This phase generally lasts less than sixty minutes.
I am fortunate to have only had a few migraines during my lifetime. My headaches always begin with visual problems, and I am unable to perform simple tasks such as opening a combination lock. I also have trouble speaking and have word-finding difficulties. The symptoms I suffer mimic a stroke.
What are the triggers of migraine headaches?
Medication Overuse Headache
Medication overuse headache (MOH) occurs when analgesics, triptans, or ergotamine agents are overused chronically. It is essential to take medications only as prescribed by your physician. There is an increased risk of MOH with opiates, Fiorinal, and analgesic medications containing barbiturates.
Medication less likely to cause MOH are hydroxyzine, metoclopramide and low-dose non-steroidal anti-inflammatory drugs such as ibuprofen and naproxen.
Medications That May Trigger a Migraine
Several drugs have the ability to trigger a migraine. These include oral contraceptives, reserpine, nitroglycerin, cocaine, nifedipine, and hydralazine.
If you suffer from migraines and are taking any of these, ask your physician for a substitute.
If you are using cocaine, either stop on your own or get treatment. Cocaine is very addictive and extremely dangerous.
Diet
Many foods are known to precipitate migraine headaches. Some of these include chocolate (I know, this is sad), processed meats, aged cheeses, onions, oranges, tomatoes, and some dairy products. Red wine and champagne consumption can also lead to migraines.
Caffeine is a double-edged sword. It can help with migraine treatment, but caffeine withdrawal can cause headaches in some individuals. For this reason, it is recommended that frequent migraine sufferers stop ingesting caffeine for a two to three month period to determine if headache frequency declines.
Individuals who consume large amounts of caffeine should slowly taper off the drug to decrease the chance of precipitating a withdrawal headache.
It is also important to be aware of additives and food preservatives. Substances such as aspartame and MSG can trigger a headache. Whole foods are always the safest option.
Environment
Cigarette smoke, perfume, weather changes, loud noises, and bright or flickering lights can cause a migraine. A change in altitude and extreme heat or cold are also culprits.
Getting too little or too much sleep can be a trigger. If possible, sleep at the same time each night for the same amount of time. Try to eat at regular intervals. Skipping meals has been shown to trigger migraines in some individuals.
Other Migraine Triggers
People with psychiatric disorders are more prone to migraines. Stress and menses also increase migraine risk.

Treatment of Migraine Headaches
It is a pretty safe bet that either you or someone you know suffers from migraine headaches. You are most likely reading this because you want to know how to make them stop!
I am going to go over abortive treatment as well as prophylactic (preventative) treatment of migraines. My goal is to present the medications with the most evidence to support their use.
Please remember that different people respond to various therapies. What works for others may not work for you. I am going to present a list of the treatments that are most likely to be effective.
Biofeedback for Migraines
During my research on migraines, I came across an article that discussed the use of biofeedback as prophylaxis for pediatric migraine headaches. Even though I am a pharmacist, I will always recommend non-drug treatments for patients if they are safe and effective.
There is not a single medication that does not possess side effects.
Biofeedback is where patients learn to control automatic bodily functions through the use of feedback such as temperature or muscle tension. When properly trained, the patient can control the temperature of their hands, for example, without the use of equipment.
When we are under stress, the blood vessels in our hands become smaller. With less blood flowing, the temperature of our hands decreases. By learning to relax using biofeedback, it is possible to lower the stress level, which increases the size of the blood vessels leading to warmer hands.
But does this work for migraines?
Nesoriuc and Martin published a meta-analysis on the effectiveness of biofeedback for migraine in 2007. They reviewed 55 studies, which included 2229 migraine patients.
The conclusion was that biofeedback significantly and substantially decreases the pain and psychological symptoms after only eleven sessions. This led to the recommendation that biofeedback can be used as an evidence-based behavioral treatment option for migraine headache prevention.
A meta-analysis looking at biofeedback as prophylaxis for pediatric migraine was conducted in 2016. The researchers concluded that biofeedback is most likely effective, especially when combined with relaxation therapy. Since the number of studies was small, and they had methodologic issues during the meta-analysis, their recommendation is to continue research on this topic.
Migraine Abortive Treatments According to the Guidelines
When you get a migraine, it can be disabling. Light, noise, and even movement can make the pain worse.
The first thing most people reach for is Excedrin migraine or ibuprofen. Excedrin migraine is acetaminophen (Tylenol) and caffeine. If this works for you great, but remember, if you get migraines often, you should avoid caffeine.
The over-the-counter medications with the best data to support use in the treatment of a migraine headache are aspirin, ibuprofen, and naproxen sodium. If these are ineffective, see your doctor.
What are the first-line treatments for migraines?
Triptan Drugs for Migraines
Triptans are first-line for migraine pain relief. There are several drugs in this class. Imitrex (sumatriptan) is the most common. Imitrex comes in a variety of dosage forms, including nasal spray, tablets, transdermal patches, and subcutaneous injection. The injection is the fastest acting and also the most effective. Remember, nausea often occurs with a migraine, so taking anything by mouth can lead to vomiting.
The triptans work by making the blood vessels in the head smaller. These drugs should NOT be used in hemiplegic or basilar migraines.
There seems to be a difference in the effectiveness of the triptans in individual patients. My advice is to see what your insurance company covers and start with that. If it doesn’t help, try another agent. The most significant difference in the individual triptans is the dosage forms available and the onset and duration of action.
Triptans available are listed below:
- Sumatriptan (Imitrex) – Injectable is ultra-fast acting and the most effective. Also available in tablets, nasal spray.
- Rizatriptan (Maxalt) – Available in disintegrating tablets and regular tablets.
- Zolmitriptan (Zomig) – Tablets, disintegrating tablets, and nasal spray
- Naratriptan (Amerge)- Slow acting/ long-lasting
- Almotriptan (Axert) – Tablets only.
- Eletriptan (Relpax) – Tablets only
- Frovatriptan (Frova): Longest acting triptan
Dihydroergotamine (Nasal Spray) for Migraines
Dihydroergotamine is available as a nasal spray (Migranol), as well as an injection that can be given intravenously, subcutaneously, or intramuscularly.
It works by constricting blood vessels. Like triptans, this medication should not be used in hemiplegic or basilar migraine.
Only the nasal spray received a level A recommendation from the American Headache Society (AHS).
The drugs in this class were the treatment of choice before the triptans were available. Ergot alkaloids such as dihydroergotamine should not be given along with protease inhibitors, macrolide antibiotics, or antifungal agents.
Ask your doctor or pharmacist if you have any questions about this.
Ergot alkaloids have many side effects, but the most common is nausea and vomiting. The nasal spray is the preferred route of administration due to less nausea.
Other Level A Recommendations for Aborting Migraines
Acetaminophen (Tylenol): Good choice for pain, especially in older individuals or those with kidney problems.
NSAIDs: Aspirin, ibuprofen, and naproxen sodium have the most evidence.
Opiates: May be useful but not recommended for chronic use. Side effects and addiction potential may outweigh benefits.
Sumatriptan/naproxen (Treximet)-A combination product promoted by the drug company.
Acetaminophen/Aspirin/Caffeine (Extra strength Excedrin)-Works very well for some but careful with caffeine.

Migraine Prevention Treatments According to Guidelines
If you experience migraine headaches often or are having to miss work on a regular basis, you may wish to take something to help prevent the headaches.
Which therapies are recommended?
Aniticonvulsants
Depakote for Migraine Prevention
Divalproex (Depakote) has substantial evidence to support its use in the prevention of migraine headaches. A Cochrane review published in 2013 found patients taking Depakote were twice as likely to decrease migraine frequency by 50% or more than those taking placebo.
Depakote does have adverse effects and risks associated with its use. It can cause congenital disabilities and should be used with caution in women of childbearing age. It also may cause weight gain, nausea, hair loss, and dizziness. Depakote has also been associated with liver failure, but this is uncommon.
Topamax for Migraines
Topamax also has a Cochrane review that supports its use in migraine prevention.
This review looked at seventeen trials and found topiramate to be two times more likely to decrease the frequency of migraines by 50% or more when compared to placebo.
Topamax can decrease appetite and commonly causes a burning or prickling sensation in the feet, arms, legs, and hands. It may also cause nausea, difficulty with memory and concentration, kidney stones, and word-finding problems.
Other Level A Recommendations to Prevent Migraines
For women who suffer from menstrually associated migraines (MAM), frovatriptan (Frova) should be offered for short-term relief.

Treatment of Nausea Occurring with Migraine
Promethazine for Migraines
Promethazine is a drug used primarily for nausea and vomiting. It can also be effective in the treatment of migraine and received a level B recommendation (probably effective) from the AHS.
This medication is available in multiple dosage forms such as tablets, injection, syrup, and suppositories. This makes promethazine useful during a migraine accompanied by nausea and vomiting.
Promethazine has the potential to be abused due to its sedative effects and its ability to cause delirium. It is also known to increase euphoria when combined with opiates.
The recreational drug “purple drank” is a mixture of promethazine with codeine, hard candy, and carbonated soft drinks.
This mixture is popular among the hip-hop culture.
Promethazine should not be used in patients with asthma.
It can cause many side effects such as nausea and vomiting, dry mouth, problems breathing, dizziness, and sedation.
Chlorpromazine for Migraines
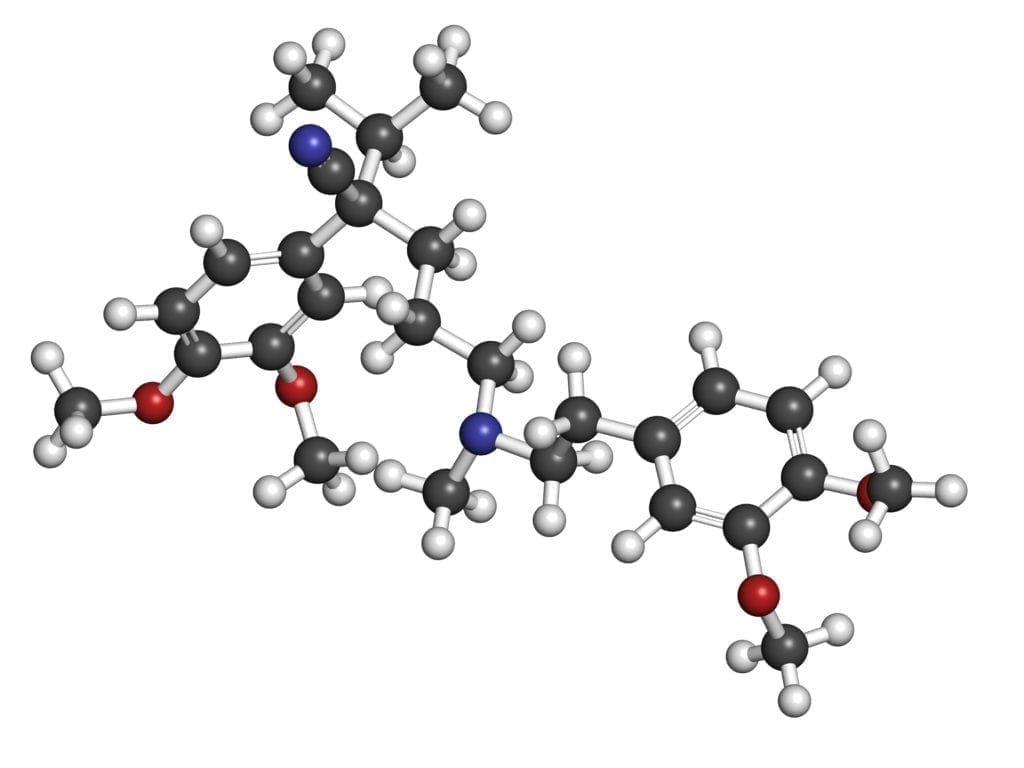
Chlorpromazine (Thorazine) is also a level B recommendation, according to the AHS. This medication is a phenothiazine that blocks dopamine receptors. This is how it works as an antipsychotic agent.
Chlorpromazine also possesses anti-nausea effects.
A study conducted in 2002 found chlorpromazine to be significantly better than a placebo in treating migraine headaches in the emergency room.
Chlorpromazine does cause a high level of sedation and postural hypotension. It is a highly anticholinergic drug leading to dry mouth, blurred vision, constipation, and confusion. It is available as a tablet and injectable form.
Droperidol for Migraines
Droperidol is also probably effective in the treatment of migraines, according to the AHS.
I have spent countless hours working in the hospital setting, and I definitely received complaints when droperidol was on back-order.
It is undoubtedly one of the favorite agents used for migraine at my institution.
Droperidol can have some pretty severe cardiac side effects. It may also cause anxiety, restlessness, and a dysphoric mood.
This drug is normally used as a pre-anesthetic agent for sedation before surgery. Droperidol has a very short duration of action.
It is only available in an injectable form.
Metoclopramide for Migraines
Metoclopramide (Reglan) is also classified as probably effective by the AHS. It is available as a tablet and as an injectable form. Reglan should not be used in patients with epilepsy. Headaches may be caused by Reglan in some individuals. Drowsiness, nausea, vomiting, and movement disorders may also occur with its use.

Alternative Migraine Treatments
There are migraine treatments available that utilize dietary supplements and other medications such as Botox. I have included some of the most popular and effective therapies below.
Botox Shots for Migraines
Botulinum toxin type A (BTX-A) was approved for the treatment of adult chronic migraine headaches in 2010.
Most of the data which led to this approval was obtained from two randomized, placebo-controlled, double-blind studies also published in 2010.
BTX-A is administered intramuscularly at a dose of 155 units once every twelve weeks. Each dose should be equally divided and administered to thirty-one specific muscle regions of the head and neck, as shown below.
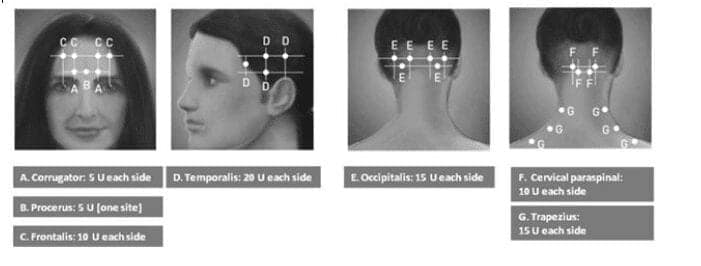
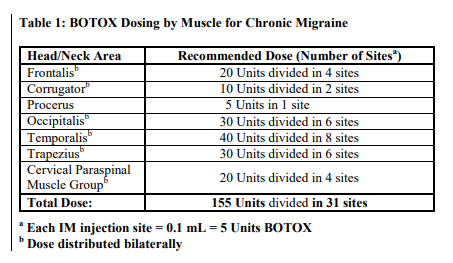
The images above were taken from the Botox package insert by Allergan, 2019
According to the American Academy of Neurology (AAN), BTX-A is safe and effective for chronic migraines and is probably effective for improving health-related quality of life (QOL) for these patients. They recommend offering BTX-A to chronic migraine sufferers to increase the number of headache-free days and improve QOL.
Chronic migraine is defined as fifteen or more headaches per month for at least three months. These headaches must last four hours or more.
The AAN recommends against the use of BTX-A for episodic migraine and considers it ineffective for this population.
An updated Cochrane systematic review was published in the British Medical Journal in 2019. This review included twenty-eight trials, which included 4190 subjects.
I prefer to cite Cochrane reviews whenever possible as they are reliable, and their evidence has the most impact on the scientific community.
They also update their studies when new information becomes available, as is evidenced in this subject.
Of the twenty-eight trials identified, twenty-three compared BTX-A with placebo injections. Three of the trials compared BTX-A with other migraine prophylactic drugs.
The studies comparing BTX-A to placebo included 23 trials with 3912 subjects. The analysis showed a reduction of 3.1 days of migraine occurrence per month in the BTX-A group.
In an episodic migraine subgroup of 418 subjects, no difference was found between the two groups.
It should be noted that BTX-A is very expensive compared to other treatment options.
It should be reserved for those with chronic migraine headaches who do not respond or cannot tolerate other therapies.
Butterbur for Migraine Headaches
Petasites hybidus, or butterbur, is a shrub that grows in wet, marshy soil. The large leaves have traditionally been used to wrap butter during warm weather to prevent melting.
This plant has been used to treat fever, cough, asthma, and wounds of the skin.
It is important to note that unprocessed butterbur contains pyrrolizidine alkaloids (uPA). These may be harmful to the liver if ingested over a prolonged period.
Butterbur, which has been processed to remove uPA is safe to consume.
There have been studies comparing butterbur to placebo.
In one study conducted in 2000, sixty men and women who suffered from a least three migraines per month were given either 50 mg butterbur extract or placebo twice daily for three months. Seventy-five percent of the butterbur group reported improvement in the number of attacks and total number of days with migraine pain, compared to only twenty-five percent of the placebo group.
Another study administered either 50 mg butterbur extract twice daily, 75 mg butterbur extract twice daily, or placebo twice daily to 202 people with migraines for three months. Patients in all three groups saw improvement in their headaches, but the 75mg butterbur group saw significant improvement as compared to the placebo group.
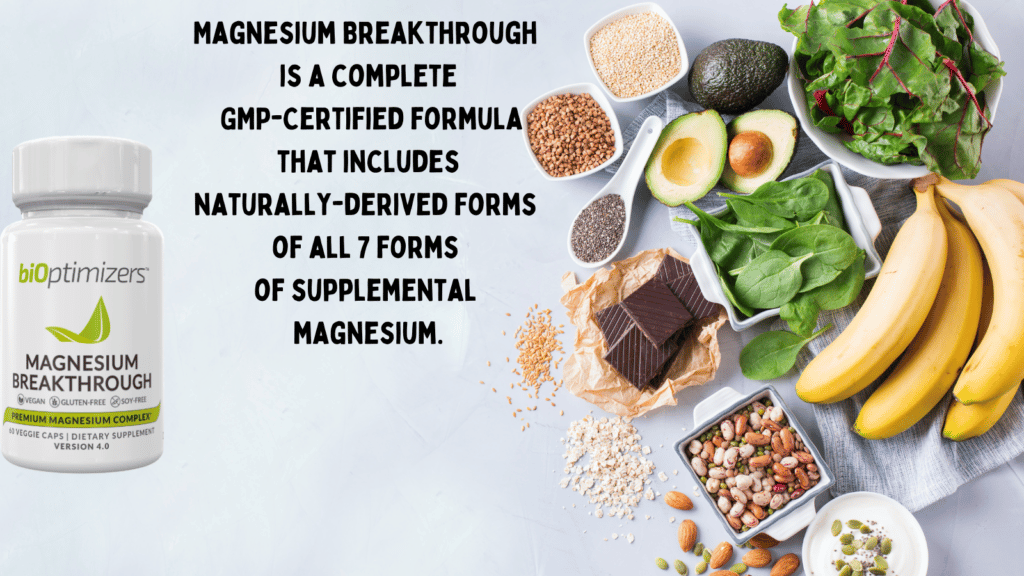
Magnesium and Riboflavin for Migraines
A meta-analysis published in 2014 compared IV magnesium with placebo in emergency room patients presenting with migraines.
Subjects received either IV magnesium, a dopamine antagonist, or a placebo.
More patients experienced pain relief in the magnesium group than in the placebo group, but it was not statistically significant.
This study also discovered magnesium works better in patients who have migraine with aura. There was no difference in effectiveness between magnesium and placebo in patients with migraine without aura.
It was also discovered that the magnesium-metoclopramide combination led to more pain relief than the placebo-metoclopramide combination.
Riboflavin has been found to be effective at reducing the number of migraines when taken at a dosage of 400 mg per day.
In a study of fifty-five patients, 400 mg of riboflavin daily was found to be superior to placebo at reducing both the number of headache days and the frequency of migraines.
The most common side effects of riboflavin are diarrhea and increased urination.
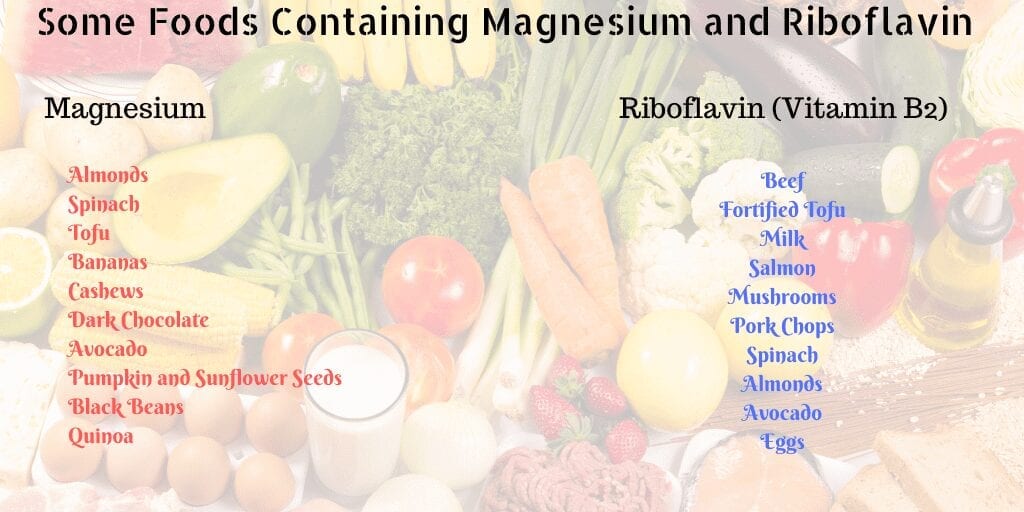
Both magnesium and riboflavin can be found in many foods:
Feverfew and Ginger for Migraines
Feverfew (Tanacetum parthenium) is a plant with flowers resembling daisies that grows wild throughout the world. This plant has previously been used for its anti-inflammatory properties and pain related to menses in women.
Tanacetum has been used to prevent migraine headaches. The flowers contain a compound known as parthenolide, which is thought to decrease the incidence of migraines utilizing multiple mechanisms of action.
Inhibition of cyclooxygenase-2, tumor nucrosis factor-alpha, interlukin-1,
and serotonin
are all thought to be involved.
A systematic review of the literature regarding feverfew and migraine was published in the Journal of Dietary Supplements in 2009.
Some interesting information was gleaned from this study. It is possible that other compounds contained in the feverfew leaves assist in parthenolide’s mechanism of action.
One of the studies found no benefit of an alcohol extract of parthenolide, while two other studies using dried leaves found a statistically significant decrease in migraine severity and frequency.
These studies found feverfew to be safe with no difference in adverse effects as compared to placebo.
It is important to note that feverfew is a supplement which is thought to prevent migraine, not treat the actual headache. For this reason, patients will be taking the supplement over an extended period.
More studies are needed to assess the long-term safety and recommended dosage of this supplement.
Can ginger fight a migraine headache?
Ginger is a common spice used in cooking. It is also used to cleanse the palate in between the consumption of various types of sushi. Ginger is native to southeastern Asia.
This plant has been used for many medical purposes, including treatment of motion sickness, generalized pain, vertigo, arthritis pain, and dyspepsia.
One study conducted in 2005 found Gelstat (an OTC drug containing ginger extract) completely alleviated migraine pain in forty-eight percent of patients within two hours.
Thirty-four percent achieved partial relief during the same period.
In a study published in May of 2013, Maghbooli et al. compared ginger to sumatriptan in the treatment of migraine headaches.
One-hundred patients were selected to either receive ginger or sumatriptan if a headache occurred.
Twenty-two percent of the sumatriptan group and twenty percent of the ginger group had a severe headache during the study and were treated.
Seventy percent of the sumatriptan group and sixty-four percent of the ginger group had their headache pain decrease by at least ninety percent two hours following drug administration.
There was not a significant difference between the two treatments regarding migraine pain relief.
The only side effect reported by the ginger group was dyspepsia. Alternatively, the sumatriptan group reported dizziness, dyspepsia, vertigo, and sedation.
Although this study had a limited number of subjects, it shows promise in ginger’s ability to fight migraine headache pain.
A dosage recommendation of 500 mg ginger taken at headache onset and repeated every four hours up to 2 grams daily for three to four days has been recommended by Mustafa and Srivastava.

Migraine headaches are a common health problem today. They lead to decreased productivity, increased health care costs, and a lower quality of life.
There are many treatments for this disorder. Choosing the right therapy depends on several factors. Patients who have nausea and vomiting occurring with their headaches may benefit from an agent that is available as a non-oral dosage form.
Elderly patients or those with kidney disease should be careful with NSAIDs. These drugs can damage the kidneys, especially if taken over a long period.
Those who suffer from multiple monthly migraine attacks may want to consider preventive drug treatment. Again, there are many options to accomplish this, and they are patient-specific.
I suggest keeping a headache journal. Write down what you eat each day, your activity level, exposure to smoke or strong odors, and hours of sleep as well as the level of stress. Try to find a pattern that leads to your headaches. It may be easier to avoid foods or other factors that cause your headaches than to use medications.
Consider biofeedback. It does take an initial time commitment but may pay off in the future if you can learn to master it.
Other alternative therapies, such as vitamins and nutraceuticals, may also decrease headache frequency. It is possible to get some of these just by eating certain foods.
More studies should be done in the future regarding these agents in the treatment and prevention of migraine.
I have covered the medications with the most evidence in this post. There are many more second and third-line agents available as well.
At times it may be necessary to combine medications to get the desired effect.
If you have any questions regarding migraine headaches or any other topic, please feel free to send me a message. I am always happy to help whenever possible.

Michael J. Brown, RPh, BCPS, BCPP
Mr. Brown is a Clinical Pharmacist specializing in pharmacotherapy and psychiatry.
Feel free to send Michael a message using this link.