- Mitchell AJ, Chan M, Bhatti H, Halton M, Grassi L, Johansen C, Meader N. Lancet Oncol. 2011 Feb; 12(2):160-74.
- Arrieta O, Angulo LP, Núñez-Valencia C, Dorantes-Gallareta Y, Macedo EO, Martínez-López D, Alvarado S, Corona-Cruz JF, Oñate-Ocaña LF. Association of depression and anxiety on quality of life, treatment adherence, and prognosis in patients with advanced non-small cell lung cancer. Ann Surg Oncol. 2013 Jun; 20(6):1941-8.
- Psychological distress and cancer survival: a follow-up 10 years after diagnosis. Brown KW, Levy AR, Rosberger Z, Edgar L. Psychosom Med. 2003 Jul-Aug; 65(4):636-43.
- Review A comprehensive review of palliative care in patients with cancer. Jaiswal R, Alici Y, Breitbart W. Int Rev Psychiatry. 2014 Feb; 26(1):87-101.
- Freedman R. Abrupt withdrawal of antidepressant treatment. Am J Psychiatry. 2010 Aug; 167(8):886-8.
- Review of pharmacological treatment in mood disorders and future directions for drug development. Li X, Frye MA, Shelton RC. Neuropsychopharmacology. 2012 Jan; 37(1):77-101.
- Ross S, Bossis A, Guss J, et al. Rapid and sustained symptom reduction following psilocybin treatment for anxiety and depression in patients with life-threatening cancer: a randomized controlled trial. J Psychopharmacol. 2016;30(12):1165-1180.
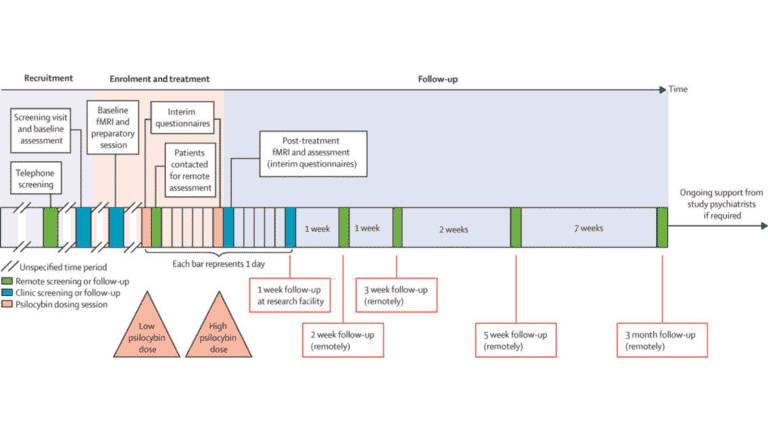
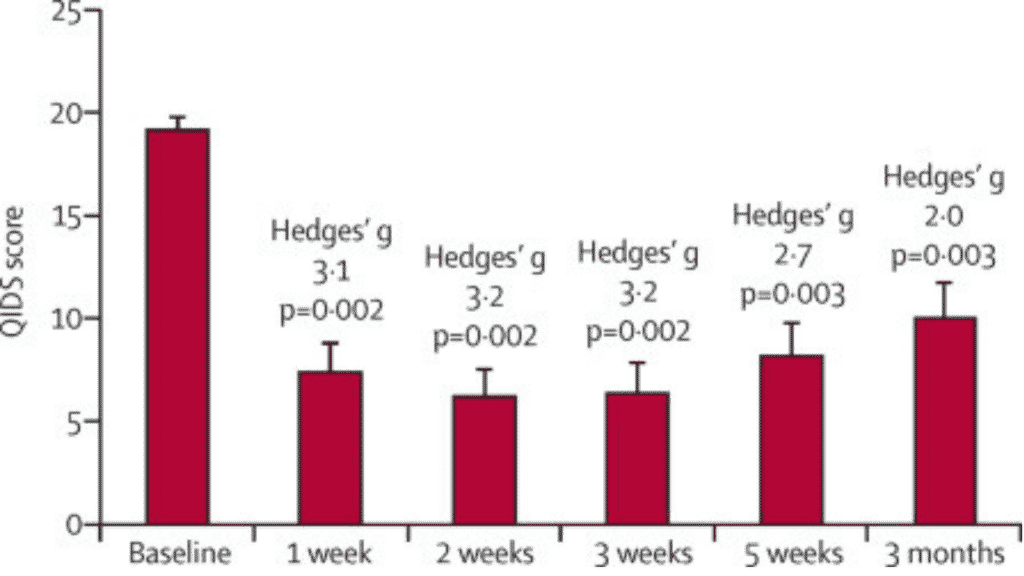
- Carhart-Harris RL, Bolstridge M, Rucker J, Day CM, Erritzoe D, Kaelen M, Bloomfield M, Rickard JA, Forbes B, Feilding A, Taylor D, Pilling S, Curran VH, Nutt DJ. Psilocybin with psychological support for treatment-resistant depression: an open-label feasibility study. Lancet Psychiatry. 2016 Jul;3(7):619-27. doi: 10.1016/S2215-0366(16)30065-7. Epub 2016 May 17. PMID: 27210031.
- Johnson MW, Garcia-Romeu A, Cosimano MP,Griffiths RR. Pilot study of the 5-HT2AR agonist psilocybin in the treatment of tobacco addiction.J Psychopharmacol. 2014; 28: 983-992.
- Bogenschutz MP, et al. Psilocybin-assisted treatment for alcohol dependence: a proof-of-concept study.J Psychopharmacol. 2015; 29: 289-299.
×
Why Choose to Autoship?
- Automatically re-order your favorite products on your schedule.
- Easily change the products or shipping date for your upcoming Scheduled Orders.
- Pause or cancel any time.